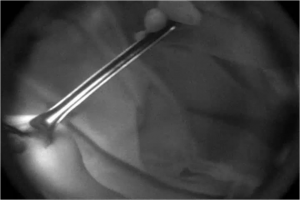
 We can see fluorescence-stained lesion through NIRF camera. Using this NIRF guidance, surgeon accurately resect the lesion, which was injected or stained before operation. Surgeon can make sure the lesion anytime during operation. Fluorescent marker can be used for non-palpable small breast cancer. Before operation, if we marks the small lesion with this novel fluorescent marker under sonography, the surgeon can see it anytime during operation.
We can see fluorescence-stained lesion through NIRF camera. Using this NIRF guidance, surgeon accurately resect the lesion, which was injected or stained before operation. Surgeon can make sure the lesion anytime during operation. Fluorescent marker can be used for non-palpable small breast cancer. Before operation, if we marks the small lesion with this novel fluorescent marker under sonography, the surgeon can see it anytime during operation.
Image from the presentation “Intraoperative Image-Guided surgery in Breast Cancer” by Seok-ki Kim, MD
Optical Surgical Navigation Interest Group Chairs:
Michael Tweedle, PhD, Ohio State University and James Basilion, PhD, Case Western Reserve University
Optical imaging can be a very powerful intraoperative tool to mark and visualize tissues, cells, and biochemical events in real time guiding the surgeon in radical resection to achieve optimal clinical results. The purpose of the WMIS Optical Surgical Navigation Interest Group OSN-IG is to help advance and support intraoperative optical molecular imaging education, innovation, standardization, and translation to clinical use.
Optical Surgical Navigation Interest Group Highlights Advancements Targeted at Improving Surgical Outcomes
The Optical Surgical Navigation Workshop, held in conjunction with WMIC 2014 showed that there is increasing momentum and excitement for this new tool. Co-organized by Professors Hyun Koo Kim of Korea University Guro Hospital, a lung cancer surgeon-scientist, James Basilion of Case Western Reserve University in Cleveland, Ohio and Michael Tweedle of Ohio State University, the workshop covered emerging molecular applications and intraoperative optical surgical navigation designed to significantly improve surgical outcomes.
Surgeons traditionally guide their hands with their eyes and sense of touch (palpation). Imaging has long guided the surgeon’s strategy, like using the results of PET and MRI scans taken days prior to the actual operation. However, optical imaging is rapidly emerging as a very powerful intraoperative tool to mark and visualize tissues, cells, and biochemical events in real time guiding the surgeon in radical resection to achieve optimal clinical results through the application of laser light, CCD cameras, light emitting chemical agents, and ultraminiaturized microscopes. Used in real time in the operating room, these technologies are collectively dubbed intraoperative imaging and surgical navigation.
The workshop was designed to cover molecular applications and instrumentation used in intraoperative optical surgical navigation and to include topics such as: clinical application, safety and efficiency, workflow, regulatory, clinical trial end points, pharmaceuticals and tissue dyes, the Optical Surgical Navigation Workshop concluded by Dr. Tweedle summarizing the likely regulatory hurdles and common sense decisions that need to be made to get these optical imaging agents through the system and into clinical practice.
Highlights of the Optical Surgical Navigation Workshop
Imaging Surgically Removed Tissue in Real-Time: Rather than waiting a week for a pathology report, researchers are investigating the ability to image surgically removed tissue in real time with a topically applied cancer cell stain to immediately inform the surgeon’s actions. “We are hopeful that our technology can reduce the ~-25% re-surgery rate in breast cancers,” noted James Basilion, Ph.D., who is developing the technology in collaboration with Go van Dam, MD, PhD, of the University of Groningen in The Netherlands.
Translational Intraoperative Optical Surgical Navigation is on the verge of executing a multitude of clinical studies conducted in Europe (using mainly antibodies and nanobodies) and several institutions in the United States. It is anticipated that within the next five years, Phase II studies will deliver the necessary data for larger multicenter studies on image-guided surgery in breast, head-and neck and colorectal cancer. Highly novel targeted nanoparticles were discussed together with the use of currently approved imaging agents to identify surgical margins in brain tumors (5-ALA) and sentinel lymph nodes (ICG) for in both lung and breast surgeries. “We also had significant presentations describing new tools for in vivo microscopic assessment of tumor margins and other biology,” said Michael Tweedle, Ph.D., whose presentation focused on overcoming the challenges researchers face in financing and lifting their discoveries through regulatory and reimbursement bureaucracies.
Optical Surgical Navigation: A number of presentations and workshop discussion groups touched on the utility of molecular imaging, including optical imaging, to manage surgical intervention for infections and its emergence as a growing emphasis for intraoperative imaging (not just about cancer). Researchers from Korea demonstrated the cutting edge in the use of ICG and 5-ALA for optical surgical navigation in humans.
To join the OSN Interest Group, click here.
Industry Perspectives
Use of Optical Probes for Infectious Disease Imaging: Imaging scientists are working to implement real-time imaging with targeted fluorescent agents that pinpoint cancer cells, then respond to applied laser light by fluorescing at a wavelength detectable by filtered CCD camera systems that can process the data and overlay the signal from the cancer- or bacteria-bound molecules onto the surgeons vision field. “You can make that signal any color you want to contrast it with the color of natural tissue” said Perkin Elmer’s Kevin P. Francis, Ph.D., who focused his lecture on infection imaging with the company’s new multichannel veterinary operating room camera that can detect several simultaneous agents emitting different wavelengths.
Novadaq Perspective
The potential for optical imaging to transform clinical practice has been the subject of much discussion between academes and industry over the past decades. But, aside from the legacy of a few non-specific dyes such as indocyanine green and methylene blue, optical imaging probes have had only limited impact in the medical field thus far. We believe however, that the field of optical imaging in medicine – fluorescence imaging in particular – is on the verge of a rapid growth period given the recent advances in chemistry, tumor biology and biophotonic technologies. For example, within the practice of clinical oncology, surgeons increasingly recognize the potential of optical technologies for the detection of residual tumors in the surgical bed. In parallel, efforts dedicated to the discovery and testing of new biomarkers have led to the development of highly specific, multifunctional cancer probes for imaging and drug delivery. Some of these molecular imaging probes are currently in Phase 1 trials. These novel imaging agents will be of most value when combined with multiplatform imaging technologies – preferably configurable for minimally invasive and open field surgery – which canintegrate pathology with anatomic and/or physiologic information through various modes of optical imaging. In this context, emerging imaging technologies with real time capabilities will play a pivotal role in surgical guidance and will have an important impact on intraoperative decision making.
We are witnessing an exciting transitional period in molecular imaging. As an increasing number of optical technologies continue to advance through developmental stages, it is almost certain that we will see some of these technologies transition into clinical practice in the next few years.
Eduardo Moriyama, PhD, Research Scientist – Imaging Agent Technologies, Novadaq
Intuitive Surgical Perspective
As the worldwide leader in robotic-assisted laparoscopic surgery, Intuitive Surgical strongly believes that optical imaging technologies will provide surgeons with the tools they need to make procedures safer and more effective.
Over 1000 of our surgical systems throughout the world have Firefly technology, enabling real-time visualization of fluorescence during surgery. Our newest surgical system, the da Vinci Xi comes with Firefly as a standard feature. When you combine this with systems from Karl Storz, Novadaq, and emerging companies such as Lumicell and Quest, one realizes that FDA-approved devices currently exist for the detection of optical agents in robotic-assisted, laparoscopic and open surgeries.
While imaging modalities such as CT, PET and MRI have done wonders for medicine, we still have issues surrounding the use of such images in the operating room due to intraoperative tissue deformation. Optical imaging solves this, as simultaneous imaging of the fluorescent and white light signals is achieved through the same endoscope, providing inherent registration of the images. From a workflow perspective, this makes the integration of the technologies extremely easy from a technical point of view, which is required for surgeon acceptance.
Exciting optical imaging agents from established companies such as Perkin Elmer, from academic groups as well as startups such as Akrotome, Blaze Biosciences, Lumicell and OnTarget Laboratories demonstrate the burgeoning interest from academics and businesses in commercializing these technologies. Nonetheless, due to difficulties surrounding the economics of imaging agents as a whole, those of us in industry and academia must find creative ways to cooperate in order to achieve these goals. Events such as the Optical Surgical Navigation Workshop organized by the WMIS are an important component of bringing us together.
Jonathan Sorger, Sr. Director of Medical Research, Intuitive Surgical
